5 Things You Should Know About Labour Induction
What happens if you don’t get into labour or if you need to have the baby earlier than planned? In these situations women may need an induction of labour (or ‘induction’ for short). There are lots of different opinions about an induction; some women ask to be induced while other women would like to avoid it as much as they can. Here are 5 things we feel are useful to know about an induction of labour.
1. Why do we recommend an induction in some women?
The most common reason for an induction is when your pregnancy is ‘post dates’. This means you haven’t had your baby yet and are over your due date. Risks to the baby increase with time and even though the risk of stillbirth is very small, this is one of the reasons we recommend all babies to be born by 42 weeks gestation.
If you have a pregnancy complication such as gestational diabetes (GDM), chances are an induction will be discussed with you, particularly when you need insulin for control. Most babies will be delivered before your due date, usually around 39 weeks gestation. Timing of delivery depends on how well your diabetes is controlled (see our blog on gestational diabetes to read more).
Other pregnancy conditions are ‘pregnancy induced hypertension’ or ‘pre-eclampsia’, these conditions usually mean that you will have your baby earlier than your due date. Many women have their babies a little later in life. If you are over 40 years of age, or needed IVF to conceive, chances are that an induction will be discussed with you too.
2. What is involved in an Induction?
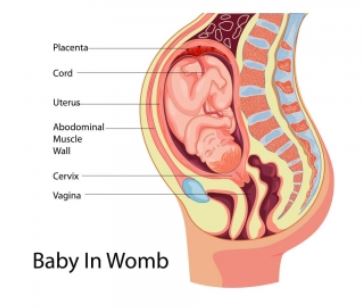
There are usually two steps in an induction. Firstly we need the cervix to become more soft, short and open (the ripening stage), and this is most commonly done with some Prostaglandin gel. The gel is inserted into the vagina where it can take its effect on the cervix. The gel can be given 3 times, 6 hours apart. A small balloon catheter inserted through the cervix is another option. This first step is usually done during the evening/night. Both methods will allow the cervix to open (dilate) enough so that we can break your waters (rupture of membranes) the next morning.
This is when the second part of the induction starts. After your waters are broken we start a hormone called Oxytocin, which will slowly bring on your contractions. This hormone is administered through a drip into your arm. It takes many hours for the contractions to become regular and strong.
If you have had a baby before, or if the cervix is already soft, short and 1-2 cm dilated, we usually skip the Prostaglandin gel and can break your waters and start the Oxytocin drip.
3. What to expect during the first part of the induction
You can expect to be admitted in the evening for Prostaglandin gel. You will stay in the Delivery Suite where the midwife will confirm the indication for induction, check that both you and your baby are well, and get you comfortable. After the gel is given, we will do a CTG (wellbeing check for the baby) and then most women tend to try and get some sleep. You are staying in the hospital and your partner can stay with you, or have a good sleep in their own bed – it’s up to you. Throughout the night the midwife will perform another vaginal examination to determine if there are any changes and whether you need a second dose of the Prostaglandin gel.
Most women will get some mild contractions after the gel. We will prescribe pain relief tablets and sleeping tablets, as we would like you to be well rested for a big day ahead.
Some women may spontaneously break their waters and proceed to get into labour. This is great and we will continue to monitor you and your baby, making sure you are both fine.
Less than 0.5% of women respond to the Prostaglandin gel very strongly and have contractions that occur too frequently. This is called “hyperstimulation” and your baby may become distressed due to these frequent contractions. If hyperstimulation occurs, most women will require a caesarean delivery ensuring a healthy outcome for the baby.
4. What happens during the second part of the induction?
The Prostaglandin has done the job and we can now break your waters. Before doing this we will again confirm your baby is still happy by doing a CTG. We will also insert an IV cannula in your arm. We break your waters by doing a vaginal examination during which we pass a thin plastic instrument that makes a small hole in the membranes. Depending on whether you’ve had a baby before and the indication of the induction, we may give you a few hours to see if the labour will start naturally. If this doesn’t happen we will start the IV drip with Oxytocin hormone. This drip will administer a very small amount of the hormone and is increased every 30 minutes to ensure regular contractions of adequate strength occur. We can increase the drip, stop or slow it down, depending on your contractions.
The second part of the induction is usually not quick, and varies between women. In general, it may take many hours before you are having some contractions at all. As the cervix is usually still a bit long and only 1-2 cm dilated the contractions will need to soften, shorten and open the cervix further. This can again take many hours. Once the cervix is around 4 cm dilated and you are having regular contractions we finally say you are “in labour”!
During your induction all pain relief options are available for you. This includes having a shower/bath, Nitrous Oxide (‘Gas’), morphine injections, and an epidural. Your midwife knows exactly what stage of the labour you are in and we recommend following their advice if you need help regarding your options for pain relief.
5. Last but not least: Inducing is safe for you and your baby!
Some women struggle with the idea of needing an induction. It is considered an intervention and may not feel natural. Some women are concerned the contractions will be too powerful and you can be worried about safety for your baby. It is important to know that an induction is safe. There is now enough evidence to support that an induction of labour does NOT increase the risk of caesarean section, instrumental delivery or adverse outcomes to you or your baby.
We hope this information is useful. If you have any specific concerns we are more than happy to discuss this during your antenatal visits.
